Before go into too much detail about IVF, I want to acknowledge that the process varies widely from person to person. As much as I was trying to avoid IVF, my protocol was fairly easy.
As a reminder, here are the steps of IVF:
Ovarian stimulation - Making your body produce lots of eggs
Egg retrieval - Taking the eggs out
Embryo creation - Fertilizing the eggs with sperm and monitoring their growth
Genetic testing (optional) - Making sure the embryos have all their chromosomes
Embryo transfer - Putting a viable embryo back inside your uterus
This section will cover through egg retrieval. If you have ever thought about freezing your eggs, you will follow this same process (just fyi, frozen embryos have a better chance surviving thaw than frozen eggs alone).
The ovarian stimulation/egg retrieval is what most people think of when they think of IVF as it is the most invasive part (i.e. definitely involves needles at multiple steps). Also, the medications in those needles are what makes IVF insanely expensive — like $4,000 if you don’t have insurance. So, you really really want these two steps to go well so you don’t have to spend money on more meds.
Ovarian stimulation
The first step is growing some eggs.
Your ovaries usually release one or maybe two eggs per month and you want to trick them into prepping 15-20 eggs using medication. Here’s extremely simplified version of egg retrieval:
You will inject yourself with medications to stimulate your ovaries to grow lots of eggs.
After a couple of days, you will start injecting a different medication to prevent the eggs from being released by your ovaries (ovulation).
You will inject yourself with one last medication to make yourself ovulate.
Exactly 35 hours after that injection, you will go in for surgery so your doctor can remove your eggs.
You will hate your life for a bit.
Ovarian stimulation is scary to people because it involves needles but the needles are tiny and you barely feel them. That said, I only had to give myself shots once a day (I had to pick a time between 7 and 10 p.m. and do it at that time every day) so I might feel differently if I had more shots.
Some people have others do their shots for them. I understand this but logistically it didn’t make sense for me. Also, if you have pets, I would keep them out of the room during your shots — there was a very frightening incident involving my cat who likes to chew on crinkly plastic and a needle package.
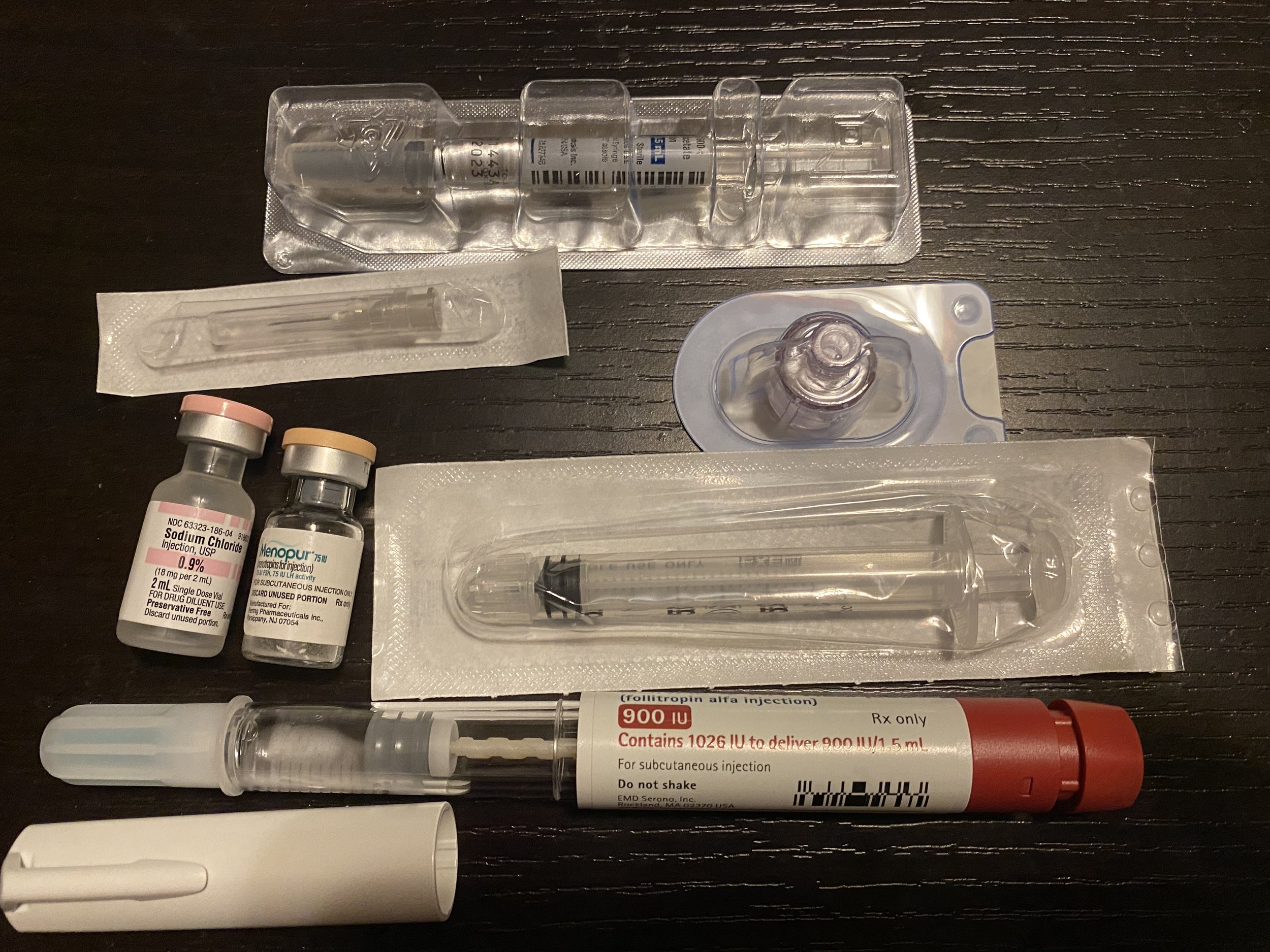
For my protocol, I had to take Gonal-F and Menopur for five days and then add in Ganirelix for five days. Gonal-F and Menopur essentially tell your body to make lots of eggs and Ganirelix tells your body not to ovulate. Gonal-F and Ganirelix were super simple — pre-filled syringes. Menopur involves some science wizardry of reconstituting a powder with diluent but you get the hang of it. Freedom Med Teach has helpful videos to learn how to administer all the different meds.
My evening routine
So yes, towards the end I had to give myself three shots every night. Then you do a trigger shot (I only had one but you might have more) and you are done with shots which is the greatest feeling! (Except lol not really but we’ll get to that later.)
During this part of IVF, you will go into the clinic every other weekday so they can take your blood to check your hormone levels and do an ultrasound and see how your eggs are developing. At this point I’d had approximately one million ultrasounds and blood draws so this was not a big deal.
If you were hoping you can drink to get yourself through the shots because you are not pregnant yet, I have some bad news for you — no drinking starting the day you begin your shots. You also have to stop physical activity and/or sex starting like Day 5 and it’s going to be a while before you can do any of that again.
My experience:
Some people have a truly awful time with the shots (bruising, they find the injections painful, etc.) but again, I was lucky here. Be sure to ice beforehand and rotate where you’re stabbing yourself every time. I think the first time I did my shots, it took 45 minutes just to mentally psych myself up to stick my abdomen with a needle twice but by the end it took 15 minutes. I dunno, you get used to it.
I was also afraid I was going to lose my shit emotionally as a result of the shots but no major change there — however, I do not generally have an emotional reaction to doses of hormones (the pill, etc.) so this might just be me.
Towards the end, I definitely felt like my ovaries were full of eggs. It wasn’t painful, but my abdomen felt bloated and I was wary of doing any activities that put my ovaries in the line of fire (i.e. I turned down watching my friend’s 95-pound dog who has a tendency to greet me via jumping). They also retrieved quite a few eggs from me so it might be different if you are growing fewer eggs.
Egg retrieval
This is surgery to remove your eggs. It is actual surgery so definitely treat it as such in terms of expectations for your recovery. Before your surgery, stock up on Gatorade or something else with electrolytes and easy-to-eat foods.
Exactly 35 hours after your trigger shot, you go in for egg retrieval. You get IV anesthesia (and an antibiotic) so you blissfully remember nothing which is great because they literally stick a needle through your vagina to get eggs out of your ovaries. Yeah, it is not fun to picture!!!
You will know how many eggs they retrieved immediately after the procedure. Your clinic will tell you that you can go back to work and most normal activities the next day but I personally think this is bullshit.
My experience:
My retrieval was at 7 a.m. and I planned to be conked out for the full day. At the surgery center, you take a Tylenol, change into your gown, get hooked to an IV, and just kind of chill until they’re ready for you. Make sure you pee beforehand, it will be the last time you can do that without pain for a while.
As with any surgery, everything happens super quickly. They wheeled me into the room, which was like, 20 degrees colder than the waiting room. I remember the lab where they made the embryos was attached to the surgery room and the door was open — I guess this makes sense so they can get the eggs over there quickly but it made me feel weird in terms of having my nether regions on full display to that team. They confirmed what surgery I was there for, my donor number, etc., and then the anesthesiologist did her thing. The last thing I remember was my doctor’s asking me to put my legs up on stirrups and me responding, “Wow I feel so ladylike.”
I woke up when I was being wheeled back into my pre-surgery room, apparently about 20 minutes later. I sat there for a little bit, they told me they got 32 eggs (which is wild but I’ll get into that next time), then I put my clothes back on and my mom drove me back home.
I was expecting to feel groggy all day, but the anesthesia wears off quickly and I felt normal by the time I got home. However, I did feel crampy and, I don’t know, like someone just stuck a needle through my vagina, so not great. I spent the day watching shitty TV, taking Tylenol exactly as often as allowed, chugging Gatorade, adjusting my heating pad, and becoming one with my couch (my mom left after lunch, leaving enough groceries for the week, which was perfect).
Mobility-wise, I could shuffle from place to place but couldn’t stand up straight. I was surprised I didn’t bleed that much, but I still felt super bloated and gained five pounds in one day from fluid retention (note that you are supposed to call your doctor immediately if it’s more than five pounds). These symptoms cleared up significantly in the next couple of days, and I was able to stop taking Tylenol by the fourth day.
The main change was that going to the bathroom (uh, both kinds) was painful, in the sense that a kind of stabbing pain alerted me to the fact that I needed to use the bathroom, followed by more stabbing when I was actually going. It stayed that way for over a week. So that was fun.
Since everyone had told me I’d be able to resume normal life the next day, I went back to work and even went to an event the night after my surgery, which is absolutely not something I would recommend to anyone (I was walking around at approximately 0.00002 mph). Plan to take two days completely off — I don’t know why this is not standard.
Also, just be aware your period is going to be real messed up after your egg retrieval. I got mine like five days after transfer (which translated to a week early). So, just when you think you’re getting over your transfer pain — here comes blood!
Next up, creating embryos.